
Revenue Cycle Management
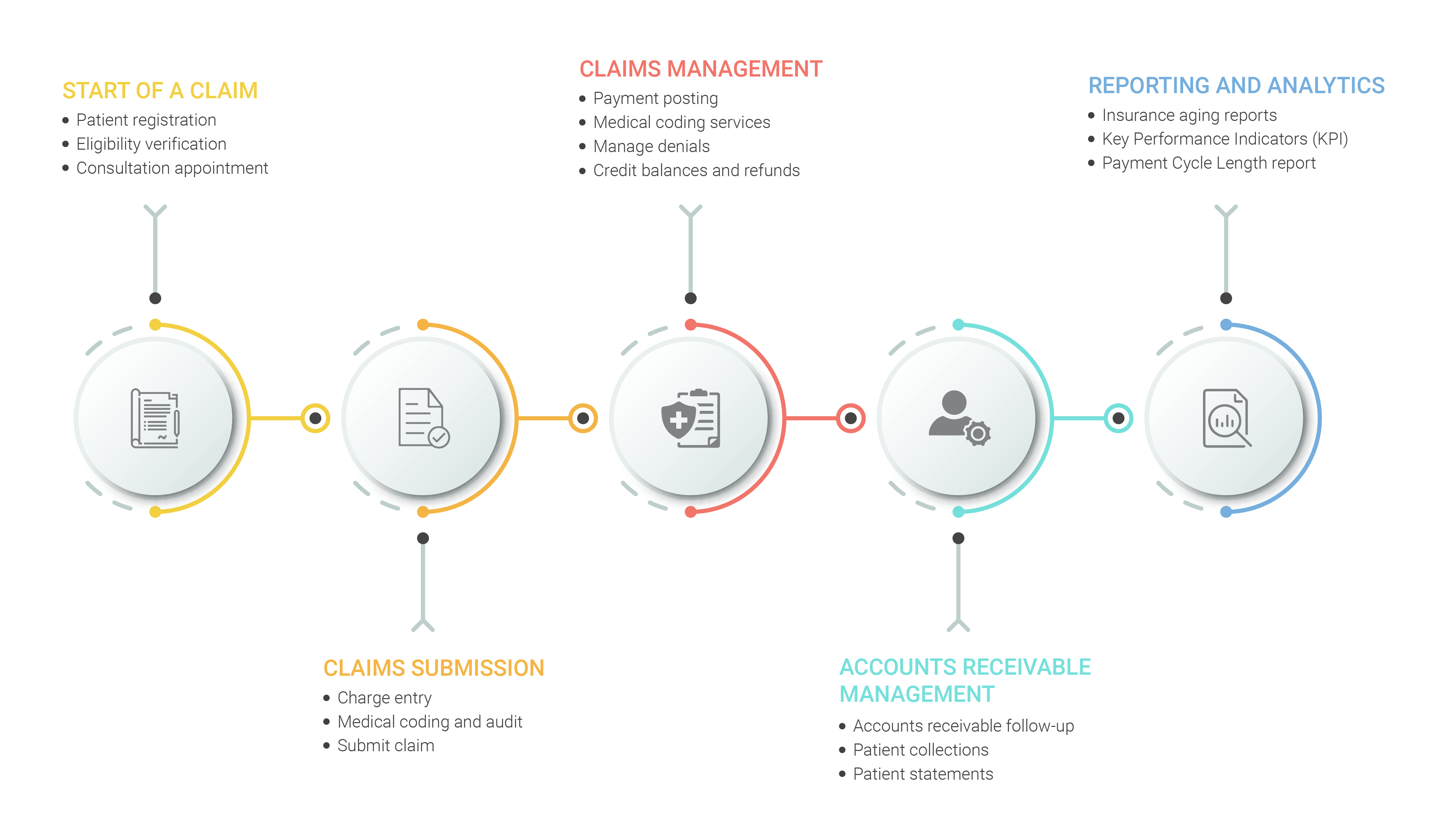
Medfields Healthcare combines intelligence and expertise with a highly specialized team of financial and clinical experts to offer a host of value-added RCM services.
The healthcare industry is undergoing a significant transformation in terms of offering holistic patient care and in maintaining financial viability. In light of these transformations, managing revenue is vital for any healthcare organization regardless of whether you are a multi-specialty hospital with multiple networks or a small healthcare network. That is where healthcare revenue cycle management shows up and this key financial process is essential for healthcare organizations to keep their doors open to treat patients.
The healthcare revenue cycle is a complex maze and the majority of healthcare organizations are under pressure in managing them efficiently amidst their stressed schedule. In order to help healthcare organizations in dealing with RCM disciplines, Medfields Healthcare offers end-to-end Revenue Cycle Management services.
Revenue Cycle Management Services We Offer
Medfields Healthcare combines intelligence and expertise with a highly specialized team of financial and clinical experts to offer a host of value-added RCM services. We ensure seamless and accurate processing by following a streamlined and integrated revenue cycle management process.
Patient Registration
Code development and continuous integration tools
Eligibility Verification
Version controls, build status and code merging
Charge Entry
Continuous testing phases which determine performance
Claims Submission
Artifact repository and application pre-deployment staging
Payment Posting
Change management, release approvals and release automation
Accounts Receivable Follow-Up
Infrastructure configuration and management
Denial Management
Applications performance monitoring and end–user experience
Credit Balances & Refunds
Applications performance monitoring and end–user experience
Self-pay review / Patient Statements
Change management, release approvals and release automation
Our Workflow

Patient Registration
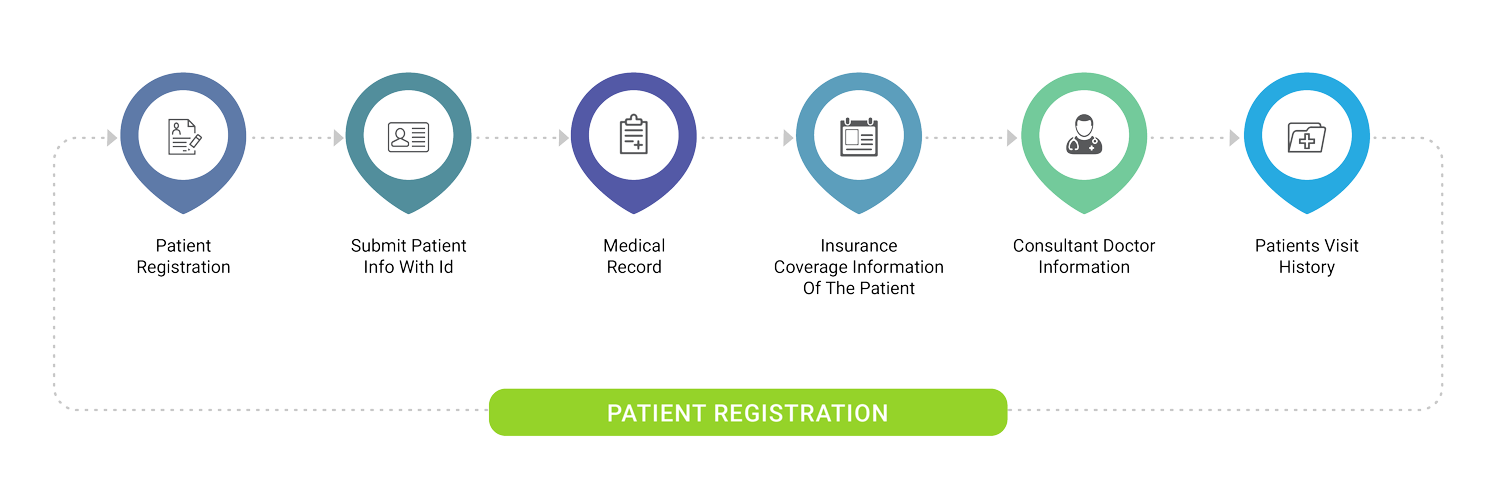
Our Patient Registration team provides a high standard service which helps you eliminate registration and billing errors that cause delays in billing and reimbursement procedures.
Like every aspect of healthcare, RCM begins with the patient. Similar to the payment and administrative aspects of healthcare, Patient’s input also plays a critical role. Getting complete and accurate patient’s information and capturing the information accurately into the revenue cycle system acts as a key success to revenue cycle management system.
Before scheduling an appointment, we collect patient demographic information, confirm patient's insurance cover and get the financial responsibility acknowledged to ensure a streamlined revenue cycle management process. Our Patient Registration team provides a high standard service which helps you eliminate registration and billing errors that cause delays in billing and reimbursement procedures. Eliminating errors and unwanted delays undoubtedly gain patient satisfaction.
What To Expect From Our Patient Registration Services?
Real-time collaboration and reporting
Enhanced productivity and accuracy
Facilitates clean claim submission

Eligibility Verification
Medfields Healthcare ensure to conduct pre-insurance verification so as to verify the eligibility regarding the particular insurance so as to speed up the payment process and reduce write-offs or bad debts
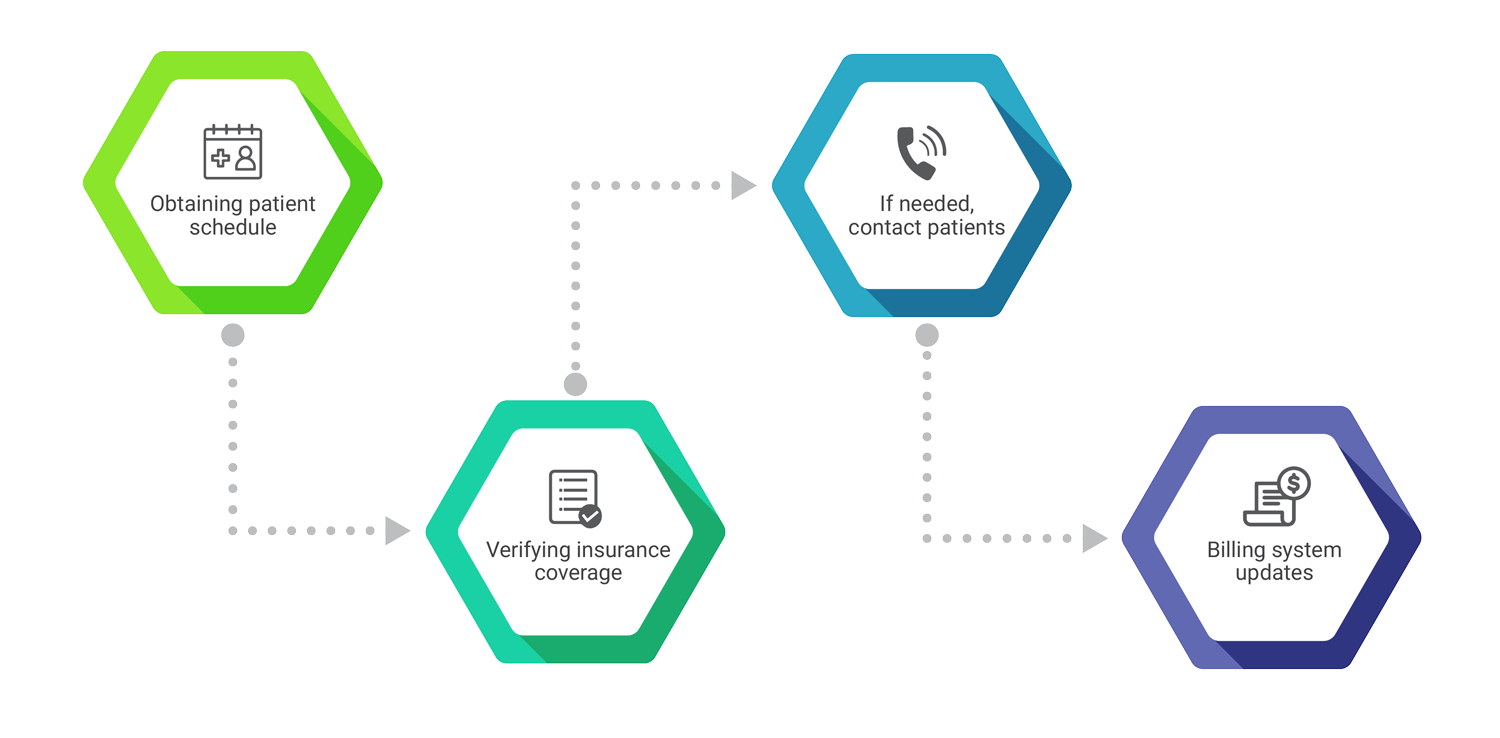
Accurate and timely determination of the patient’s eligibility is much needed to gather precise information regarding the patient’s insurance coverage. Such eligibility verification checks deliver an explicit view on patient's coverage, out-of-network benefits, and detailed insurance information.
Before the patient's visit to the healthcare provider, we ensure to conduct pre-insurance verification so as to verify the eligibility regarding the particular insurance. Our pre-insurance verification includes the following
- Checks if there are any requirements for pre-authorization or referral
- If the patient has met the deductible, we check the amount of co-insurance the patient shares
- Checks if any copayment has to be collected
- Finally, we ensure that if the patient's insurance, covers the service sought from the provider
Majority of the insurance providers do not provide retro authorization, hence eligibility verification is very much needed as it speeds up the payment process and reduced write-offs or bad debts.
What To Expect From Our Eligibility Verification Services?
Enhanced patient satisfaction
Cash flow optimization
Minimize patient-related denials
Eliminates claim rejections by payers due to lack of accurate information

Charge Entry
Medfields Healthcare offers charge entry services that yield superior accuracy and decreased deficits. Our charge entry experts are capable of processing a huge volume of charge entry transactions with exceptional accuracy.
Revenue leakages can happen if efficient care is not put up for information documentation. In order to accomplish a sustainable improvement in the overall process, effective collaboration should be maintained between coding and charge entry teams.
Medfields Healthcare offers charge entry services that yield superior accuracy and decreased deficits. Our charge entry experts are capable of processing a huge volume of charge entry transactions with exceptional accuracy. We perform an audit on the entered charges before submission and ensures a clean claim is submitted to the insurance. During charge audit, we perform the following actions
- Confirm charges with diverse department billers and coders
- Comparing charges by patient’s accounts
- Detect duplicate charges, undercharges and overcharges
- Check if all treatments are rendered
What To Expect From Our Charge Entry and Audit Services?
Improved productivity and accuracy by optimizing revenue and identifying missed revenue
Instances of over-billing, coding errors, and missed charges are identified during charge audit
Avoids delay in AR processing and fix compliance issues for charge overages

Claims Submission
Our categorized style of passing on claims to specific employee groups based on pro-actively identified measures maximizes the efficiency of the claim submission process.
Medfields Healthcare also offers claim submission services to help the physicians rationalize their claims management. Our categorized style of passing on claims to specific employee groups based on pro-actively identified measures maximizes the efficiency of the claim submission process.
In general, clearing houses provide a report within 24 hours. This report contains accepted and rejected claims on the submitted list. Our team will review these reports on a priority basis. We will fix the rejected claims and resubmit them to the insurance providers within 24 hours. We also possess the capability of processing paper claims.
What We Offer?
Health plan comprises of huge volumes of claims on a daily basis and we perform the following for Claims processing.
What To Expect From Our Claims Submission Services?
Minimized turn around and appeal times
Lower administrative costs
A Decrease in overall claim operation costs

Payment Posting
Medfields Healthcare provides a streamlined payment posting workflow for insurance and patient payments and insights on clinical documentation and coding processes and effectiveness of your front-end patient collections.
Payment posting is a resource-intensive task and a good payment posting team is responsible for the overall effectiveness of the revenue cycle process. Medfields Healthcare provides a streamlined payment posting workflow for insurance and patient payments. Our payment posting team do not just process payments, they provide insights on overpayment, denial, underpayment made. We also provide insights on clinical documentation and coding processes and effectiveness of your front-end patient collections.
If you have electronic lockboxes, we can interface with them to get EOB’s. If you are receiving paper EOB’s, you only need to scan and send them to Practice Management Software (PMS) and we can work on it. We will ensure that all the payments are posted and reconciled within 24 hours.
We offer the following Payment Posting services
- Analytic inputs on denials, underpayment, and overpayment
- Denial handling
- Knowledge management
- Filing claims with secondary payers
- Policy development for write-off and adjustments

Accounts Receivable Follow-Up
Our dedicated A/R team follows-up with the insurance provider to resolve denied claims. Appropriate actions are taken to receive maximum reimbursement from the insurance companies by reopening them.
The accounts receivable follow-up team plays a crucial part as there are chances for the claims to get denied if they don’t adhere to the rules. Our dedicated A/R team follows-up with the insurance provider to resolve denied claims. Appropriate actions are taken to receive maximum reimbursement from the insurance companies by reopening them.
With our executive leadership team and highly skilled AR specialists, we proactively strategize the approach of denials received from payers. Our team will also work on fixing the clustered denials permanently to avoid delayed payments in future claims.
We strategize A/R follow-up through 3 phases
What To Expect From Our A/R Follow-up Services?
Recovery of overdue payments
Quick follow-up for denied claims
Recovery of claims with pending information
Reduced time for outstanding accounts

Denial Management
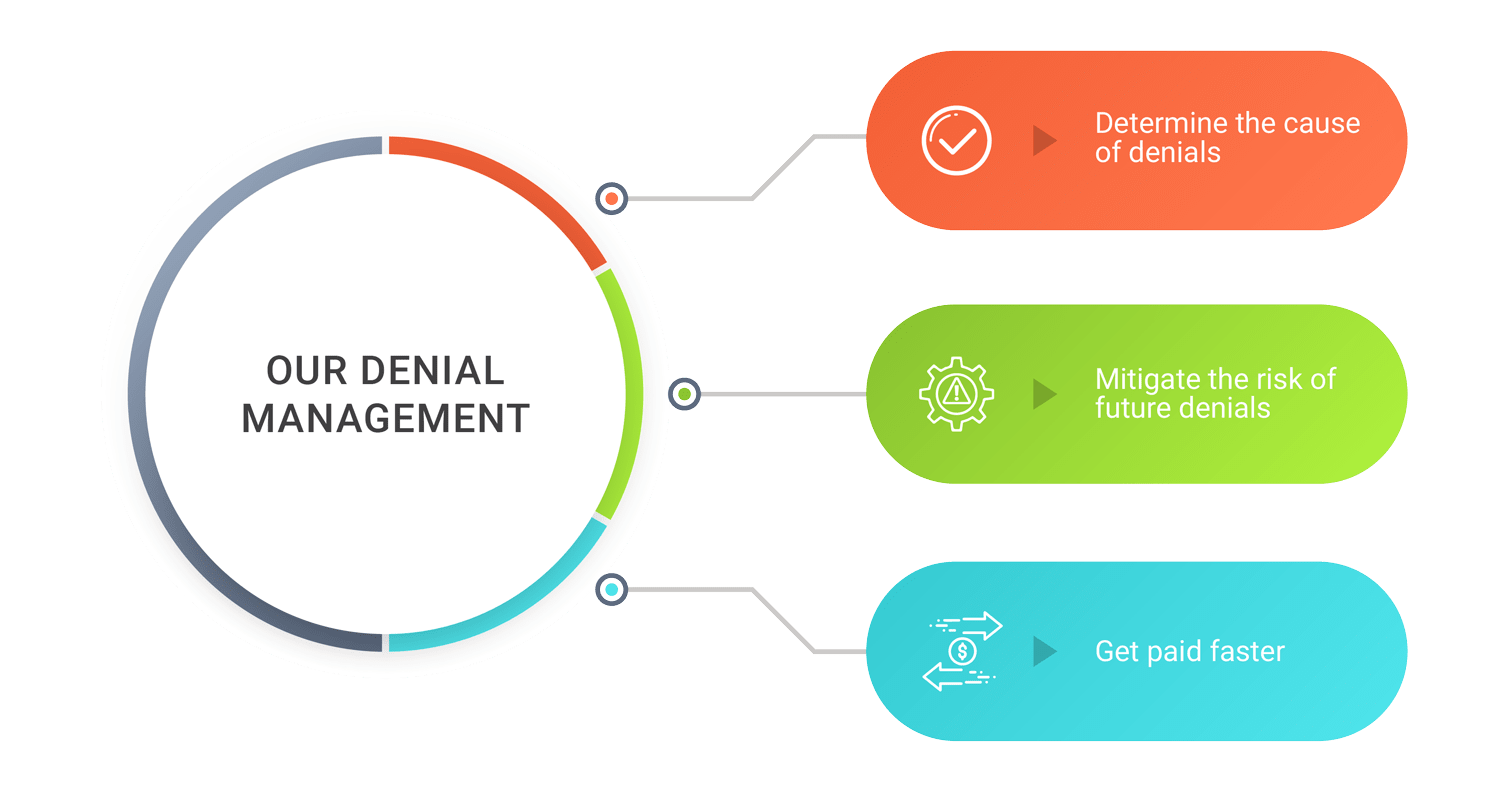
We aim at the highest possible reimbursement on the claims. We help you maximize the success at collecting payments for denied / underpaid claims. Our systematic appeal process aggressively pursues reimbursement from contracted payers.
Dealing with medical claim denials is a time-consuming task and it’s a critical element in successful revenue cycle management. We follow a systematic, hands-on approach to deal with denied claims. As a first step, we analyze each claim and determine the best course of action. Secondly, we prioritize the claims based on patient demographics or business rules to ensure maximum benefits. Then, we take steps to prevent future denials by enhancing the billing practices in your healthcare.
Our denial management strategies include
- Stratify, categorize the denials through our denial management system
- Build denial management tactics customized as per client circumstances/needs
- Categorize the denials by payer, root cause and other unique factors
- Execute strategic approaches for optimistic appeals and reversal of denials

Credit Balances & Refunds
Hashroot Healthcare follows a two-tier review system for credit balances and refunds. Our credit balances and refund services will help you improve patient satisfaction, insights, and loyalty.
Hashroot Healthcare follows a two-tier review system for credit balances and refunds. Our dedicated credit balance team will begin with reviewing the credit balance reports, identifying insurance or patient refunds. As a next step, the Quality Assurance team will review the identified refunds and initiate refunds with supporting documents involving all the respective parties in a timely manner. Our credit balances and refund services will help you improve patient satisfaction, insights, and loyalty.
Our credit balance and refund services focus on the following

Self-pay review / Patient Statements
Our self-pay review experts understand how critical it is to bill a patient, we ensure that a complete reconciliation of the patient payments before initiating a patient statement as per requirements (weekly/monthly), Further follow-up is performed through patient calls.
Reports
As a complement to our clients, Medfields Healthcare offers its reporting package for free. Our package contains detailed dashboards focusing on each sub-product we serve you, customized reports including insurance aging reports, Key Performance Indicators (KPI) report and payment cycle length report. It offers a detailed view of your practice's financial health. Our reporting capabilities and specialized analytics help your practice perform most granular level analysis for trends.
